Is Chronic Fatigue Syndrome (ME/CFS) a Brain Disease? The 2016 IACFS/ME Conference Pt. III
 Remember: $100,000 Year End Matching Gift Opportunity: A generous donor will match your gift to Simmaron between now and December 31, 2016, doubling your impact!Chronic fatigue syndrome (ME/CFS) may be many things: an autonomic nervous system disease, or a disease involving the mitochondria, or an immune disease, but the IACFS/ME conference made one thing crystal clear - this disease effects the brain. Given the recent metabolomic findings suggesting that a low energy or hypometabolic state is present it makes sense that the most energy intensive organ of all - the brain - might be affected. Plus, recent evidence suggesting that the brain's immune system may be particularly affected suggests that brain might just be where it all comes together for ME/CFS.In Part III of our 2016 IACFS/ME Fort Lauderdale Conference Overviews check out what the Conference told us about brain in chronic fatigue syndrome (ME/CFS).
Remember: $100,000 Year End Matching Gift Opportunity: A generous donor will match your gift to Simmaron between now and December 31, 2016, doubling your impact!Chronic fatigue syndrome (ME/CFS) may be many things: an autonomic nervous system disease, or a disease involving the mitochondria, or an immune disease, but the IACFS/ME conference made one thing crystal clear - this disease effects the brain. Given the recent metabolomic findings suggesting that a low energy or hypometabolic state is present it makes sense that the most energy intensive organ of all - the brain - might be affected. Plus, recent evidence suggesting that the brain's immune system may be particularly affected suggests that brain might just be where it all comes together for ME/CFS.In Part III of our 2016 IACFS/ME Fort Lauderdale Conference Overviews check out what the Conference told us about brain in chronic fatigue syndrome (ME/CFS).
- The IACFS/ME 2016 Conference Overviews #1: Energy and Exercise To the Fore
- Is Chronic Fatigue Syndrome An Inflammatory Disease? The 2016 IACFS/ME Conference Overviews Pt. II
Dr. Natelson: The Bad News / Good News Presentation
Dr. Natelson was in surprisingly good spirits given that he was delivering what must have been some wrenching news. His recent study indicated he could kiss about a decade of work and one really interesting hypothesis goodbye.A number of his studies had suggested that ME/CFS patients without mood disorders had more brain abnormalities (MRI's, spinal taps, neuropsychological testing, lactate levels) than ME/CFS patients with mood disorders. It was an unexpected and exciting finding that was backed up by several studies, but the crucial larger study found no difference at all.It's certainly a cautionary tale regarding the small, generally underpowered studies that permeate this disease. Dr. Newton appears to have gone through a similar process; a stream of publications on muscle and mitochondrial issues were unfortunately later negated by a larger follow up study. It shows we can't count on findings until they're nailed down by bigger studies.The news wasn't all bad. Natelson's latest study validated the fact that the major antioxidant in the brain - glutathione (GSH) - is lower in ME/CFS (we can accept that finding) and ventricular lactate levels are higher than in healthy controls (we can accept that one as well). Both findings would seemingly fit in well with studies showing that aerobic energy production is blunted and that neuroinflammation is present. (We can't accept the neuroinflammation finding yet.)Dr. Natelson, a neurologist, believes pro-inflammatory cytokines are probably whacking glutathione in ME/CFS. He also believes that reduced cerebral blood flows are a solid finding.Occult Patients. About half the ME/CFS patients in his study also had two or more brain abnormalities - a condition Natelson called an "occult encephalopathy". Occult refers to hidden or concealed abnormalities that take special tests to uncover. Encephalopathy is a broad term that refers to a syndrome that affects brain functioning. Natelson, then, has evidence (in what appears to be a fairly large study) that a hidden brain disorder is present in about half the ME/CFS patients.Now that Natelson has evidence that a brain encephalopathy is present in about half the ME/CFS patients, he hopes to use proteomics to find a biomarker in the cerebral spinal fluid (CSF). He's preparing a grant proposal. This won’t be his first go-around in the proteomics field. Natelson was the senior author of the 2011 Schutser proteomics study which cast doubt on the idea that chronic Lyme disease is a subset of ME/CFS.Natelson has high hopes for proteomics - a technology that he believes will help uncover unique biomarkers. In fact, Natelson, neurologist that he is, believes the hunt for a biomarker should begin in the cerebral spinal fluid, and then move to the blood. Because ME/CFS is, more than anything, a brain disorder, the best biomarkers are going to show up in the fluid that bathes the brain. They're present in the blood too, but are being obscured by all the other factors in the rich broth that the blood is. His plan, then, is to locate them in the CSF and then find them in the blood.
POSTER - Zeineh Replicates Stanford Study
Zeineh's arcuate fasiculatus results made a big, big splash when they came out in 2014. It was just a small pilot study, but it was Stanford, and that was enough for media outlets from CNN to Bloomberg News, the San Francisco Chronicle, and WebMD to lead with the news that ME/CFS is real.
I vividly remember Dr. Hyde, who knows of what he speaks regarding brain imaging, standing up at the Stanford Symposium and saying that was the best presentation on brain imaging in ME/CFS he had ever seen.The Zeineh findings were exciting for a number of reasons. One, Zeineh used cutting-edge imaging technology called diffusion tensor imaging (DTI) that had not been used in ME/CFS before. (One of the benefits of working at Stanford, Zeineh stated, was access to the best technology in the world.) We've always hoped that as medical testing gets more precise it will uncover issues that haven't been seen before, and that's what happened here.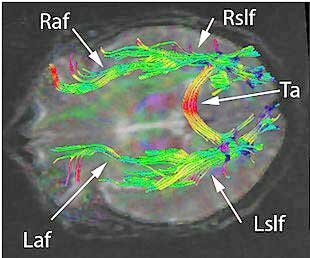 We know that the gross nerve damage present in multiple sclerosis isn't present in ME/CFS, but we also know that the Simmaron Research Foundation's cerebral spinal fluid study suggests that immune issues in ME/CFS patients’ brains may be almost as severe as those in MS patients. Zeineh examined the brain's microstructure, and his findings suggested that atrophy in the wiring that connects the different sections of our brain together had occurred. That kind of damage would impede the free flow of signals across the brain - making it more difficult to think and process information. (Many brain diseases are now considered primarily diseases of connectivity.)After his first study was released Zeineh pointed to its potential importance stating
We know that the gross nerve damage present in multiple sclerosis isn't present in ME/CFS, but we also know that the Simmaron Research Foundation's cerebral spinal fluid study suggests that immune issues in ME/CFS patients’ brains may be almost as severe as those in MS patients. Zeineh examined the brain's microstructure, and his findings suggested that atrophy in the wiring that connects the different sections of our brain together had occurred. That kind of damage would impede the free flow of signals across the brain - making it more difficult to think and process information. (Many brain diseases are now considered primarily diseases of connectivity.)After his first study was released Zeineh pointed to its potential importance stating
“Most CFS patients at some point in time have been accused of being hypochondriacs and their symptoms dismissed by others. And there is still skepticism in the medical community about the diagnosis. That’s one of the reasons these findings are important.” – Michael Zeineh
Zeineh's findings also suggested reduced white matter and problems with the thalamus and basal ganglia were present. He attributed the fasiculatus results to inflammation.Leptin Again.....Not only did Zeineh replicate his past results, but his ability to correlate them (in a preliminary analysis) with cytokine levels suggested that inflammation was indeed responsible for the damage he found. The real surprise, though, was the cytokine that popped up; it was leptin. With all the different cytokine results floating around (See the IACFS/ME Conference Immune blog) it was shocking to see a familiar cytokine pop up - and leptin at that.Nobody had connected leptin to ME/CFS until Jarred Younger's Good Day /Bad Day study suggested a couple of years ago that it was driving the immune problems in ME/CFS. (Younger is in the middle of a larger validation study now.) Younger believes that leptin could play a key role in the neuroinflammation believed to be present in chronic fatigue syndrome. Now Zeineh's (preliminary) analysis suggests that leptin may be causing the brain injury he's found. Although these results are preliminary, these are the kind of results this field could really use.Zeineh has moved fast; he published his first study in 2014 and he presented the results of this study in 2016.
POSTERS: The Zinn's Damaged Connectome
Talk about connectivity: the Zinn's and Lenny Jason's latest study found problems with connectivity in spades in what must be one of the most damaged brain networks of all in ME/CFS - the attention network. (Talk about a good fit for fatigued, concentration-challenged ME/CFS patients.) The Zinn's found that the different brain-wave bands in this network were not in sync; while two were increased, another was decreased. Their small study also found significantly increased activation of three brain-wave bands in the attention network during a task relative to healthy controls. That actually wasn't good news; it suggested that ME/CFS patients had to work VERY hard to maintain their attention during that task.Connectivity issues came to the fore in the Zinn's next poster as well. We know that information processing is slowed in ME/CFS. We also know that different regions of the brain have to work together to process information. Put those together and it raises the possibility that the slowed information processing in chronic fatigue syndrome could be the result of bad connections. Again, the Zinn's small study suggests it just might be. Their EEG results pinpointed one brain-wave band that was inhibited across the occipital (rear), parietal (top) and temporal (front) lobes (i.e. a good chunk of the brain). Even worse the signaling "hubs" most effected in ME/CFS constituted "the most electrically active" regions of the brain.A regression analysis also suggested that the longer you've had this illness the less well connected these parts of the brain are. The Zinns referred to their findings as "widespread functional dysregulation in the connectome".At the conference, Marcie Zinn pointed out someone vigorously talking to a group clustered around their posters. "That's Rex Cannon”, she whispered. It turns out he actually wrote THE BOOK on the type of EEG analysis they’re doing. The Zinn's and Lenny Jason had apparently invited him down to the conference and he was interested; in fact he was so interested in their findings that they're now collaborating with him.
Again, the Zinn's small study suggests it just might be. Their EEG results pinpointed one brain-wave band that was inhibited across the occipital (rear), parietal (top) and temporal (front) lobes (i.e. a good chunk of the brain). Even worse the signaling "hubs" most effected in ME/CFS constituted "the most electrically active" regions of the brain.A regression analysis also suggested that the longer you've had this illness the less well connected these parts of the brain are. The Zinns referred to their findings as "widespread functional dysregulation in the connectome".At the conference, Marcie Zinn pointed out someone vigorously talking to a group clustered around their posters. "That's Rex Cannon”, she whispered. It turns out he actually wrote THE BOOK on the type of EEG analysis they’re doing. The Zinn's and Lenny Jason had apparently invited him down to the conference and he was interested; in fact he was so interested in their findings that they're now collaborating with him.
Byron Hyde - the Pioneer
The "father" of brain imaging research in ME/CFS, Bryon Hyde, didn't present but he was there and provided a nicely illustrated booklet on his findings. Hyde said he had a new book coming out on ME/CFS soon.Hyde has been using SPECT scans to diagnose and treat patients for decades; his experience indicates that hypo perfusion or low blood flows to different parts of the brain is common in ME/CFS. Furthermore be believes that low blood flows to certain parts of the brain are causing many of the major problems in ME/CFS. Simply by assessing a SPECT scan he can probably tell you what kind of patient you are.In the booklet he demonstrated how he's able to tie certain SPECT scan findings to distinct problems ME/CFS patients face.
- Autonomic dysfunction - patients with autonomic dysfunction always, in his experience, demonstrate reduced blood flows in an area above the insular cortex called the operculum. The insula regulates homeostasis; e.g. the autonomic nervous system. Damage to this area is associated with orthostatic intolerance, blood vessel problems and problems with heart regulation.
Hyde, long associated with ME/CFS and critical of exercise therapies, is able to find middle ground with regard to activity. The damage to the insula and therefor to the autonomic nervous system is too significant, he believes, for these patients to benefit from graded exercise therapy (GET), but he also believes that patients shouldn’t let fear keep them in bed forever either. Depending on how severely ill a person is, Hyde states that "a gradual, patient regulated increase in activity is necessary, both for the body and the soul".
- Muscle dysfunction - Patients with muscle dysfunction show low blood flows to the motor cortex (Brodman's area 4 of the posterior lobe).
- Cognitive problems - Patients’ problems with information processing (which included everyone), speech comprehension, and processing visual and auditory information - all have left anterior temporal lobe injuries. These are found in all ME patients.
- Lots of Stuff - Patients with problems in a host of areas including learning, complex motor skills (driving?), sleep, alertness, multi-tasking, emotions, etc. demonstrate low blood flows to the anterior and posterior cingulate lobes. Most patients have injuries in both these areas.
Hyde believes the 1984 Incline Village/Lake Tahoe outbreak investigated by the CDC was a classic enterovirus epidemic. He asserts in the booklet that Stephen Straus’ blockage of a publication about this outbreak in the New England Journal of Medicine by Dr. Peterson and others had tragic consequences. Hyde believes that pure ME is an enteroviral disease diagnosed using disease history, gastric or GIT biopsy and a SPECT scan.If Hyde is right about enteroviral infections, some hope may be on the horizon. Enteroviral infections are so difficult to treat given our limited pharmocopia that most doctors don't even test for them. Hyde reported, though, that several new enteroviral drugs (Pirodavir, Vapendavir, Pocapavir, Plecoaril and Rupintivir) are in the early stages of being tested.Hyde has a new book coming out on ME soon.
Brain Research Heating Up!
 Interest in neuroinflammation in chronic fatigue syndrome (ME/CFS) is growing, and that means more emphasis on the brain. The problems Natelson and Shungu have described (increased lactate, decreased glutathione and reduced cerebral blood flows) are likely the result of increased inflammation and oxidative stress. At the IACFS/ME conference Dane Cook demonstrated that exercise not only impairs cognition a day later but that it also puts a whopping damper on ME/CFS patients’ brain activity.After Zeineh's mighty diffusion-tensor machine uncovered microstructural damage in one of the main connective pathways in the brain, his preliminary analyses suggest that inflammation (via leptin) was the cause. Meanwhile, different issues with "the connectome" in the brain showed up in the Zinn's (soon to be published) studies. Their tagging of the alertness network made perfect sense.The brain research is heating up! Quite literally. The Solve ME/CFS Initiative just funded Jarred Younger's attempt to assess neuroinflammation in the brain using a new heat scanning technique. Younger believes areas of the brain associated with fatigue are going to be red hot (figuratively speaking) in ME/CFS patients.All these interesting results mean an increased interest in examining our best gateway to the brain (short of a biopsy): the cerebral spinal fluid (CSF). As was noted, Dr. Natelson is eager to get underway with his pro
Interest in neuroinflammation in chronic fatigue syndrome (ME/CFS) is growing, and that means more emphasis on the brain. The problems Natelson and Shungu have described (increased lactate, decreased glutathione and reduced cerebral blood flows) are likely the result of increased inflammation and oxidative stress. At the IACFS/ME conference Dane Cook demonstrated that exercise not only impairs cognition a day later but that it also puts a whopping damper on ME/CFS patients’ brain activity.After Zeineh's mighty diffusion-tensor machine uncovered microstructural damage in one of the main connective pathways in the brain, his preliminary analyses suggest that inflammation (via leptin) was the cause. Meanwhile, different issues with "the connectome" in the brain showed up in the Zinn's (soon to be published) studies. Their tagging of the alertness network made perfect sense.The brain research is heating up! Quite literally. The Solve ME/CFS Initiative just funded Jarred Younger's attempt to assess neuroinflammation in the brain using a new heat scanning technique. Younger believes areas of the brain associated with fatigue are going to be red hot (figuratively speaking) in ME/CFS patients.All these interesting results mean an increased interest in examining our best gateway to the brain (short of a biopsy): the cerebral spinal fluid (CSF). As was noted, Dr. Natelson is eager to get underway with his pro teome CSF study. Dr. Baraniuk is currently examining the exosomes - small fluid vesicles that contain inflammatory factors - in the CSF of ME/CFS patients to see if they're adding to the inflammatory milieu there. The Simmaron Foundation's new spinal fluid study, which is incorporating Dr. Naviaux's metabolomic results, aims to duplicate and expand on its past CSF study.
teome CSF study. Dr. Baraniuk is currently examining the exosomes - small fluid vesicles that contain inflammatory factors - in the CSF of ME/CFS patients to see if they're adding to the inflammatory milieu there. The Simmaron Foundation's new spinal fluid study, which is incorporating Dr. Naviaux's metabolomic results, aims to duplicate and expand on its past CSF study.
That study showed a degree of immune dysfunction almost equal to that found in multiple sclerosis. Remarkably, almost half the cytokines in the ME/CFS patients were abnormal. No exercise was needed to tweak them. There was no need to filter for duration or severity either. Even at rest those cytokines were off, off, off. That suggested that major and readily identifiable immune issues exist in the brain. It also suggested, as Dr. Natelson proposed, that the brain might just be the first place researchers should go to look for immune problems in ME/CFS.Given the variable cytokine results often seen in this field, it was stunning to see the Simmaron Foundation's CSF cytokine results essentially duplicate those found in the Lipkin/Hornig blood study. That got Ian Lipkin so excited that he flew all the way to Incline Village to promote it last year. Simmaron is raising money for that project right now.