Is Chronic Lyme Disease - Not Lyme Disease At All?
Is Chronic Lyme Disease (CLD) actually Lyme disease? That's one of the questions asked during the Simmaron Research Foundation's Patient Day in September.It was a full room in beautiful Incline Village sitting on the northern shore of Lake Tahoe in Nevada. Emily Taylor of SMCI came up from LA, Gunnar took time off from medical school. Maureen Hanson and Mady Hornig flew over from the East Coast; Dr. Konstance Knox from the Midwest. The locals included Anita Patton, Courtney Miller, Eric Johnson, and, of course, there was Dr. Peterson. Why some people who have been treated for Lyme disease remain ill is a knotty question, and it has pertinence for chronic fatigue syndrome (ME/CFS). Both in Lyme disease and chronic fatigue syndrome (ME/CFS) many people become and then remain ill after an infection. Why that happens is a mystery.Some people think that chronic Lyme disease is simply another subset of chronic fatigue syndrome; that the Borrelia burgdorfii infection which ticked off chronic Lyme disease is no different from the herpesvirus or enteroviral or other infection that just happened to send ME/CFS patients' systems into a tailspin. The idea is that it's not the infection, it's the fact that an infection occurred. That's what the Dubbo and other studies which have shown that ME/CFS can be triggered by a large of number of pathogens suggest.Others believe that the Borrelia infection is still there, deeply hidden, but grinding away in the chronically ill.No one knows, but the idea that different pathogens are causing similar issues in ME/CFS and Lyme is belied by a study which found significantly different proteins in the cerebral spinal fluid of ME/CFS and Lyme disease.Dr. Konstance Knox believes the two diseases may, in fact, be very different. In her Simmaron Patient Day presentation, she suggests a pathogen may be present in chronically ill Lyme disease patients but not the Borrelia bacteria; she believes that a tick-borne virus called the Powassan Deer Tick virus, which at its worst is fully as dangerous as Borrelia or more, may be doing its work.
Why some people who have been treated for Lyme disease remain ill is a knotty question, and it has pertinence for chronic fatigue syndrome (ME/CFS). Both in Lyme disease and chronic fatigue syndrome (ME/CFS) many people become and then remain ill after an infection. Why that happens is a mystery.Some people think that chronic Lyme disease is simply another subset of chronic fatigue syndrome; that the Borrelia burgdorfii infection which ticked off chronic Lyme disease is no different from the herpesvirus or enteroviral or other infection that just happened to send ME/CFS patients' systems into a tailspin. The idea is that it's not the infection, it's the fact that an infection occurred. That's what the Dubbo and other studies which have shown that ME/CFS can be triggered by a large of number of pathogens suggest.Others believe that the Borrelia infection is still there, deeply hidden, but grinding away in the chronically ill.No one knows, but the idea that different pathogens are causing similar issues in ME/CFS and Lyme is belied by a study which found significantly different proteins in the cerebral spinal fluid of ME/CFS and Lyme disease.Dr. Konstance Knox believes the two diseases may, in fact, be very different. In her Simmaron Patient Day presentation, she suggests a pathogen may be present in chronically ill Lyme disease patients but not the Borrelia bacteria; she believes that a tick-borne virus called the Powassan Deer Tick virus, which at its worst is fully as dangerous as Borrelia or more, may be doing its work.
The Powassan Deer Tick Virus
The Powassan Tick-borne virus was first isolated from a person from Powassan, Canada in 1958. (Powassan, like Lyme, Connecticut, is another small town that just happened to get stuck with the name of a disease.) The Powassan virus is a Flavivirus related to such nasties as Zika, Dengue, West Nile Virus, and tick-borne encephalitis virus (TBEV). All these viruses can cause brain swelling (encephalitis).The scariest thing about the Powassan virus is how quickly it can be transmitted. Because the Borrelia bacteria that causes Lyme is carried in the stomach of a tick, the tick has to feed for quite a while before the bacteria actually makes into humans. Because the Powassan virus, on the other hand, is carried in the saliva of the deer tick, it takes a mere 15 minutes or so for it to jump from a feeding tick into your bloodstream. A Powassan infected tick can jump on, feed for a bit - transmit the virus - and then jump off, without you ever knowing it. Since ticks are so small and POWV transmission so rapid, few patients with Powassan encephalitis recall their tick bites.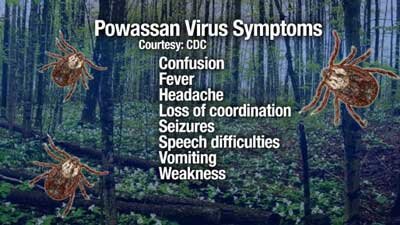 Most people infected with Powassan Virus (POWV) experience flu-like symptoms such as headache, sore throat, drowsiness and disorientation. If the infection spreads to the brain, the virus can cause everything from lethargy, high fevers, vomiting, respiratory problems and difficulty speaking to paralysis, seizures, coma and even death.Powassan-triggered encephalitis is accompanied by the infiltration of lymphocytes and monocytes into the brain and the widespread destruction of neurons in the motor areas of the brainstem (affecting movement), the cerebellum, basal ganglia (potentially affecting movement again) and the thalamus. MRI's pick up only non-specific abnormalities and thus are not diagnostic but suggest that brainstem may be particularly effected.Studies on Powassan infections are rare but some suggest that no less than fifty percent of Powassan survivors may be left with permanent neurological problems including partial paralysis, headaches, memory impairment and/or paralysis of the eye muscles.A 2015 paper presenting eight verified cases of neuroinvasive Powassan virus infection in New England bore this out. Two of the patients died, four fairly quickly recovered and two exhibited from medium to long-term problems. One 21 year old man who entered the hospital with vomiting, fever and confusion was given methylprednisolone and IVIG. He improved over time and left the hospital alert, oriented, and "speaking in short sentences". He was unable to return to work for seven months. Fifteen months later, a 52 year old man still had persistent headaches as well as problems with motor functioning and coordination.Because surveillance of the Powassan virus has been poor, it’s difficult to estimate its true incidence in humans. Luckily, far more ticks carry the Borrelia bacteria (20-50% of ticks in endemic areas) than carry the Powassan virus (1-10%). Unluckily, the Powassan virus appears to be spreading.After Powassan virus caused the sudden death of a Massachusetts woman, a tick surveillance program found from 0-16% of ticks in a given area carried the virus. A Canadian survey suggested that 3% of residents of Ontario province in Canada had been exposed to the virus. These surveys suggest far more people have been exposed to the virus than suspected. Most undoubtedly experienced symptoms similar to those of a mild cold. Others who were more seriously affected probably never got tested for Powassan.Much of what we know about the Powassan virus comes from study of a closely related virus in the Europe and Asia called Tick-borne encephalitis virus which causes thousands of neurological illnesses every year. Studies on the Powassan were almost non-existent until around 2011 when the research started picking up. Powassan virus is considered a "rare but severe neuroinvasive disease".Could Chronic Lyme Disease Caused by the Powassan Virus?
Most people infected with Powassan Virus (POWV) experience flu-like symptoms such as headache, sore throat, drowsiness and disorientation. If the infection spreads to the brain, the virus can cause everything from lethargy, high fevers, vomiting, respiratory problems and difficulty speaking to paralysis, seizures, coma and even death.Powassan-triggered encephalitis is accompanied by the infiltration of lymphocytes and monocytes into the brain and the widespread destruction of neurons in the motor areas of the brainstem (affecting movement), the cerebellum, basal ganglia (potentially affecting movement again) and the thalamus. MRI's pick up only non-specific abnormalities and thus are not diagnostic but suggest that brainstem may be particularly effected.Studies on Powassan infections are rare but some suggest that no less than fifty percent of Powassan survivors may be left with permanent neurological problems including partial paralysis, headaches, memory impairment and/or paralysis of the eye muscles.A 2015 paper presenting eight verified cases of neuroinvasive Powassan virus infection in New England bore this out. Two of the patients died, four fairly quickly recovered and two exhibited from medium to long-term problems. One 21 year old man who entered the hospital with vomiting, fever and confusion was given methylprednisolone and IVIG. He improved over time and left the hospital alert, oriented, and "speaking in short sentences". He was unable to return to work for seven months. Fifteen months later, a 52 year old man still had persistent headaches as well as problems with motor functioning and coordination.Because surveillance of the Powassan virus has been poor, it’s difficult to estimate its true incidence in humans. Luckily, far more ticks carry the Borrelia bacteria (20-50% of ticks in endemic areas) than carry the Powassan virus (1-10%). Unluckily, the Powassan virus appears to be spreading.After Powassan virus caused the sudden death of a Massachusetts woman, a tick surveillance program found from 0-16% of ticks in a given area carried the virus. A Canadian survey suggested that 3% of residents of Ontario province in Canada had been exposed to the virus. These surveys suggest far more people have been exposed to the virus than suspected. Most undoubtedly experienced symptoms similar to those of a mild cold. Others who were more seriously affected probably never got tested for Powassan.Much of what we know about the Powassan virus comes from study of a closely related virus in the Europe and Asia called Tick-borne encephalitis virus which causes thousands of neurological illnesses every year. Studies on the Powassan were almost non-existent until around 2011 when the research started picking up. Powassan virus is considered a "rare but severe neuroinvasive disease".Could Chronic Lyme Disease Caused by the Powassan Virus? Simmaron Scientific Board member and collaborator, Konnie Knox has been leading a recent surge in research publications on the Powassan virus. Her recent survey of the Ixoides scapularis ticks known to carry Lyme disease and Powassan virus in Wisconsin found that 5% carried the Powassan virus. Rather ominously half of the ticks carrying Lyme disease also carried the Powassan virus.With Lyme disease fairly common in Wisconsin (@ 187 cases/100,000) Knox's finding strongly suggested that Powassan infections were being under-reported in Wisconsin. (If Knox's findings are validated, then Powassan virus infections probably occur on the order of at 90 cases per 100,000 in Wisconsin, or as much as 5400 cases per year.)Next, Knox tested 95 patients seen at a clinic for possible Lyme disease over four months in 2015 in northern Wisconsin. Lyme disease, POWV, West Nile virus (WNV), Tick-borne encephalitis virus, V, yellow fever virus, dengue viruses 1–4, and Japanese encephalitis virus were tested for.
Simmaron Scientific Board member and collaborator, Konnie Knox has been leading a recent surge in research publications on the Powassan virus. Her recent survey of the Ixoides scapularis ticks known to carry Lyme disease and Powassan virus in Wisconsin found that 5% carried the Powassan virus. Rather ominously half of the ticks carrying Lyme disease also carried the Powassan virus.With Lyme disease fairly common in Wisconsin (@ 187 cases/100,000) Knox's finding strongly suggested that Powassan infections were being under-reported in Wisconsin. (If Knox's findings are validated, then Powassan virus infections probably occur on the order of at 90 cases per 100,000 in Wisconsin, or as much as 5400 cases per year.)Next, Knox tested 95 patients seen at a clinic for possible Lyme disease over four months in 2015 in northern Wisconsin. Lyme disease, POWV, West Nile virus (WNV), Tick-borne encephalitis virus, V, yellow fever virus, dengue viruses 1–4, and Japanese encephalitis virus were tested for. Serologic evidence of POWV infection was present in 10% of the patients and confirmed in 3% of them by other testing. Almost half of the patients with an acute Borrelia infection were infected with the Powassan virus. When the patients with a validated Powassan infection were tested, 87% were also found to be infected with Lyme disease. None, fortunately, had signs of a neuroinvasive disease.The fact that 10% of Lyme patients come down with Chronic Lyme Disease and, Knox's findings suggest that about 10% of patients with Lyme disease may also be infected with the Powassan Virus, is of course, more than intriguing.Could chronic Lyme disease or ME/CFS patients be suffering from a unusual, untreated infection? Knox's present research into ME/CFS patients could help answer that question. Knox will be testing several hundred ME/CFS patients for evidence of Lyme Disease, Powassan virus, and other tick and insect-borne diseases.
Serologic evidence of POWV infection was present in 10% of the patients and confirmed in 3% of them by other testing. Almost half of the patients with an acute Borrelia infection were infected with the Powassan virus. When the patients with a validated Powassan infection were tested, 87% were also found to be infected with Lyme disease. None, fortunately, had signs of a neuroinvasive disease.The fact that 10% of Lyme patients come down with Chronic Lyme Disease and, Knox's findings suggest that about 10% of patients with Lyme disease may also be infected with the Powassan Virus, is of course, more than intriguing.Could chronic Lyme disease or ME/CFS patients be suffering from a unusual, untreated infection? Knox's present research into ME/CFS patients could help answer that question. Knox will be testing several hundred ME/CFS patients for evidence of Lyme Disease, Powassan virus, and other tick and insect-borne diseases.
Lyme Disease Or ?
- Konstance Knox who owns a diagnostic laboratory, noted that Lyme testing has improved and that good Lyme testing is not impossible. (She liked the CDC protocol which calls for a two-step testing process.) She's confident in the results from her lab which uses machine testing rather than subjective human testing to assess the test results.
She noted that one of the biggest problems with Lyme diagnosis is getting tested too early. Because it takes about four weeks for the Lyme immune factors to show up in the blood, the tests aren't accurate until you've been infected for about a month.The Lyme diagnosis question, of course, is a big one. Get it wrong, as the story of one ME/CFS patient in the audience indicated, and you could be in for years of expensive treatments which leave you worse off. After a diagnosis based on neurological and non-specific symptoms, a CD 57 test, and a negative Western blot test from Igenex, this patient had been on and off antibiotics for about five years. Talking to her later she said she'd improved tremendously on antibiotics at times, but the treatment ultimately failed and left her worse off than ever. (She suspected that the anti-inflammatory effects of the antibiotics had temporarily helped.)She would be in the chronic Lyme disease category except for the fact that she never have had Lyme disease in the first place. In fact, her symptoms didn't really fit. She'd marveled at other "Lyme patients" who were able to exercise. Despite the fact that she'd visited a clinic that treated complex, chronic diseases, she didn't know that her main symptom - post-exertional malaise - was the defining characteristic of ME/CFS until she visited an ME/CFS clinic last year.Knox suggested that a lot of putative "Lyme" patients may not be Lyme patients at all. She's found, for instance, a very low incidence of Lyme disease in Dr. Peterson's patients, many of whom probably hail from the Western United States. She did, however, find evidence of a tick borne virus in about 11% of a 200 patient sample.
Conclusion
People who still suffer from the symptoms of Lyme disease after being appropriately treated for it are a medical mystery. Some doctors believe the Lyme bacteria is still present. Others believe that the Lyme infection may have triggered an ME/CFS-like condition. Simmaron Research Foundation Board member and collaborator, Dr. Konstance Knox, believes some people with chronic Lyme disease may be suffering from an unidentified Powassan virus infection transmitted by the same tick.Powassan virus is a poorly studied virus that can be quickly transmitted by ticks. While most people probably pass off the virus quickly, a neuroinvasive infection can cause serious symptoms including paralysis, stroke, coma and even death.Dr. Konstance Knox's studies suggest that Powassan virus is often present in ticks harboring the Borrelia bacteria that causes Lyme disease, and that about 10% of Lyme disease patients have been exposed to the virus. That's an intriguing finding given that about 10% of Lyme patients come down with chronic Lyme disease.Dr. Knox is currently studying the incidence of the Lyme disease bacteria, Powassan virus and other insect vectors in Dr. Peterson's chronic fatigue syndrome (ME/CFS) patients. Stay tuned...