The Brainstem, Vagus Nerve, Neuroinflammation and Chronic Fatigue Syndrome: The VanElzakker Way
 In 2013, Michael VanElzakker produced one of the most intriguing hypotheses to date in ME/CFS. His Vagus Nerve Hypothesis proposed that an infection/inflammation near the vagus nerve was causing it to send an unending stream of messages to the brain, telling it to essentially shut the body down by producing fatigue, pain and other symptoms. Since then, he’s been particularly interested in the connection between the vagus nerve, the brainstem and the ME/CFS.He's not the only one interested in the brainstem. In 2019 once his brainstem compression was alleviated, Jeff completely recovered from his severe ME/CFS, POTS and MCAS. Since he published his story over a dozen people have been diagnosed with craniocervical instability - a condition which compresses the brainstem.In this critical review paper, VanElzakker et. al. pick apart some of the research done and provide a guide to successfully getting at the brainstem and other regions of the brain. It's called a "Critical Review" and is critical, indeed. It finds many past ME/CFS studies wanting, but then points a way to a better possible future. If brainstem problems play a role in ME/CFS these researchers demonstrate how to get at them.http://simmaronresearch.com/2013/12/one-theory-explain-vagus-nerve-infection-chronic-fatigue-syndrome/
In 2013, Michael VanElzakker produced one of the most intriguing hypotheses to date in ME/CFS. His Vagus Nerve Hypothesis proposed that an infection/inflammation near the vagus nerve was causing it to send an unending stream of messages to the brain, telling it to essentially shut the body down by producing fatigue, pain and other symptoms. Since then, he’s been particularly interested in the connection between the vagus nerve, the brainstem and the ME/CFS.He's not the only one interested in the brainstem. In 2019 once his brainstem compression was alleviated, Jeff completely recovered from his severe ME/CFS, POTS and MCAS. Since he published his story over a dozen people have been diagnosed with craniocervical instability - a condition which compresses the brainstem.In this critical review paper, VanElzakker et. al. pick apart some of the research done and provide a guide to successfully getting at the brainstem and other regions of the brain. It's called a "Critical Review" and is critical, indeed. It finds many past ME/CFS studies wanting, but then points a way to a better possible future. If brainstem problems play a role in ME/CFS these researchers demonstrate how to get at them.http://simmaronresearch.com/2013/12/one-theory-explain-vagus-nerve-infection-chronic-fatigue-syndrome/
Neuroinflammation and Cytokines in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Critical Review of Research Methods. Michael B. VanElzakker, Sydney A. Brumfield and Paula S. Lara Mejia. Front. Neurol., 10 January 2019 https://doi.org/10.3389/fneur.2018.01033 https://www.frontiersin.org/articles/10.3389/fneur.2018.01033/full
First, VanElzakker et. al. examines one of the sacred cows in the chronic fatigue syndrome (ME/CFS) community - the preferred term for so many: myalgic encephalomyelitis (ME), which refers to muscle pain (myalgia) related to central nervous system inflammation (encephalomyelitis).While muscle pain is common, it's not universal. Even people with severe ME may not report pain.Still, the core part of the definition deals with central nervous system inflammation - a description that, with the emergence of the 2015 Yakatomi and the 2019 Younger studies, seems more and more likely to stick. (A 2018 PET scan study also found neuroinflammation in fibromyalgia as well.)The idea that inflammation plays a key role in this illness makes sense, given the infectious trigger so commonly (but not universally) found. The authors are just a few among many (Avindra Nath, Jarred Younger, Andrew Lloyd and others) who believe that an infectious event has triggered changes in the brain that are producing fatigue, pain and other problems in ME/CFS.They point to three ways an infectious trigger could produce central nervous system inflammation in ME/CFS:A) immune factors (e.g. cytokines) triggered by the infection could get transported across the blood-brain barrier (BBB) that protects the brain. The normally taut blood–brain barrier makes blood-borne infections of the brain rare, but it can, like the gut, become leaky in inflammatory states, allowing immune factors and pathogens entry. Once in the central nervous system, they could trigger a large inflammatory response, orB) High concentrations of immune factors could allow pathogens to passively diffuse across the BBB, orC) Immune factors in the blood could trigger the vagus nerve to send signals to the brainstem and brain, which then sparks an inflammatory response.It’s the last option that primarily concerns these authors. VanElzakker is the author of the Vagus Nerve Hypothesis, which proposes that an infection/inflammation near the vagus nerve is causing it to send an unrelenting stream of signals to the brain, telling it to produce the flu-like symptoms that constitute "sickness behavior" (withdrawal to bed), which isolates infected people from the community and keeps them from spreading an infection.The largest nerve in the body, the vagus nerve transmits sensory, autonomic, immune and other signals to the brainstem - making it potentially a key player in a possible neuroinflammatory disease like ME/CFS.Studies indicate that inflammation in the periphery tends to produce a mirror inflammatory response from the immune cells (the glia) in the brain. Even small levels of cytokines in the periphery or body have the potential to activate the chemoreceptors in the vagus nerve, which then activate the immune system in the brain.That brain activation, interestingly, tends to occur in regions (basal ganglia, limbic system organs (amygdala, hippocampus and hypothalamus), anterior cingulate cortex, prefrontal cortex, and thalamus), which studies suggest are also involved in ME/CFS.
The Brainstem
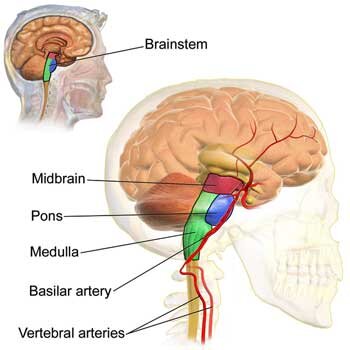 The authors believe the brainstem (which, as it name implies, is found at the very base of the brain, above the termination of the spinal cord), could play a key role in chronic fatigue syndrome (ME/CFS) for four reasons:
The authors believe the brainstem (which, as it name implies, is found at the very base of the brain, above the termination of the spinal cord), could play a key role in chronic fatigue syndrome (ME/CFS) for four reasons:
- Immune signals from the vagus nerve to the brain travel through the brainstem.
- The brainstem is dense with mast cells, and mast cell activation syndrome (MCAS) appears to be common in ME/CFS.
- The brainstem regulates autonomic nervous system functioning - a common trouble area for ME/CFS and related disorders.
- The brainstem also regulates immune functioning; in particular, it triggers an anti-inflammatory response that should limit the inflammatory response.
Whether caused by a structural problem (as in Jeff's case), inflammation or an infection, the brainstem is a centrally placed brain component that produces many of the issues in ME/CFS.https://www.healthrising.org/blog/2019/02/27/brainstem-compression-chronic-fatigue-syndrome-me-cfs-fibromyalgia-pots-craniocervical-instability/
Seeing the Brainstem in Chronic Fatigue Syndrome (ME/CFS)
Consistent inflammation of the brainstem has not, however, been found in ME/CFS. The authors argue, though, that researchers have rarely used the right kind of imaging needed to investigate this.The most commonly used method for measuring inflammation in the brain involves measuring the 18kD translocator protein (TSPO) with a PET scan. This protein is produced when the immune cells of the brain - the microglia - become activated. Because the microglia are the chief producers of inflammation in the brain, the TSPO provides a reliable way to indirectly measure neuroinflammation and its effects.
The Nakatomi Study
Nakotomi's small ME/CFS study using TSPO made a big splash in 2014. Tony Komaroff called the finding of central nervous system inflammation the most important study in decades. Five years later, Van Elzakker et. al. called it "important" and potentially "groundbreaking". The study used TSPO imaging to find widespread neuroinflammation, particularly in the areas leading from the brainstem to the thalamus.While the authors regard Nakatomi's study as potentially groundbreaking, the study is not without significant issues. The authors, in fact, seemed a bit shocked that Nakatomi found as many effects as he did, given the techniques used.The neuroimaging techniques Nakatomi used (and which most researchers use) were not designed to address brainstem inflammation. Nakatomi used a spatial "registration" technique that aligns the image on the neocortex or upper part of the brain. This kind of alignment is typically done because researchers tend to focus on the upper, "higher" functioning areas of the brain. It can, however, impair the sensitivity of imaging done on the lower, more densely packed, primitive areas of the brain, such as the brainstem, and lead to false negatives. Nakatomi also used an older tracer (PK-11195) which does not penetrate deeply into the brain and can bind to unintended elements in the brain. Differences in blood-brain barrier permeability between the ME/CFS patients and healthy controls - a distinct possibility - could have confounded the results, as well. Nakatomi's use of the cerebellum as a kind of baseline measure could have introduced further issues if problems with the cerebellum (another possibility) exist in ME/CFS.Plus, the hypometabolism believed present in ME/CFS could have resulted in lower amounts of the tracer being metabolized than usual - causing higher amounts of the tracer to reach the brain - and producing a false positive. Because exercise may affect how much of the tracer is taken up into the cells, Nakatomi's use of healthy, non-sedentary controls instead of sedentary controls introduced another issue.Finally, because the brainstem actually pulses with every heartbeat, that movement needs to be accounted for - and usually isn't in ME/CFS studies. The very small but important nuclei in the brainstem are also often not picked up with the standard imaging techniques used in ME/CFS research.Nakatomi's study results make sense given what we know, and were given a sort of validation by Jarred Younger's recent results using thermal mapping - a new technology - but we need more validation.The takeaway is that the brainstem - because of the role it plays in autonomic nervous system functioning, immune regulation and the transmission of motor signals - could play a major role in ME/CFS, but is essentially, according to these authors, still something of a black box.
Nakatomi also used an older tracer (PK-11195) which does not penetrate deeply into the brain and can bind to unintended elements in the brain. Differences in blood-brain barrier permeability between the ME/CFS patients and healthy controls - a distinct possibility - could have confounded the results, as well. Nakatomi's use of the cerebellum as a kind of baseline measure could have introduced further issues if problems with the cerebellum (another possibility) exist in ME/CFS.Plus, the hypometabolism believed present in ME/CFS could have resulted in lower amounts of the tracer being metabolized than usual - causing higher amounts of the tracer to reach the brain - and producing a false positive. Because exercise may affect how much of the tracer is taken up into the cells, Nakatomi's use of healthy, non-sedentary controls instead of sedentary controls introduced another issue.Finally, because the brainstem actually pulses with every heartbeat, that movement needs to be accounted for - and usually isn't in ME/CFS studies. The very small but important nuclei in the brainstem are also often not picked up with the standard imaging techniques used in ME/CFS research.Nakatomi's study results make sense given what we know, and were given a sort of validation by Jarred Younger's recent results using thermal mapping - a new technology - but we need more validation.The takeaway is that the brainstem - because of the role it plays in autonomic nervous system functioning, immune regulation and the transmission of motor signals - could play a major role in ME/CFS, but is essentially, according to these authors, still something of a black box.
Barnden's Brainstem - the Australian Study
It's not completely a black box, though. Researchers using other techniques have found evidence of brainstem problems in ME/CFS. Barndem in Australia, in particular, has done a series of MRI studies which have found striking brainstem issues in ME/CFS.(During his talk at the 2019 Emerge conference, Barnden noted how he had to shift his MRI to avoid the alignment problem (that VanElzakker mentioned) which prevented him from getting a good image of the brainstem. )One study found that reduced brainstem grey matter volume - suggesting that damage to the neurons in the brainstem had occurred - was correlated with autonomic nervous system problems in ME/CFS.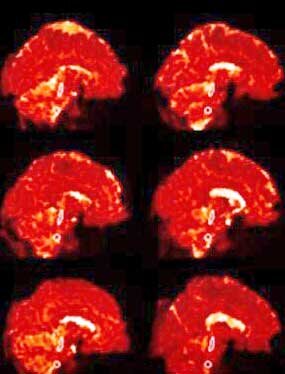 Another study finding of impaired communication from the brainstem nuclei to other nuclei in the brain suggested the same, and found increased signs of myelination in the sensorimotor cortex of the brain. Barnden proposed that decreased signaling from a damaged brainstem provoked a compensatory increase in myelination in the sensorimotor region as it bulked up to try to understand the limited signaling coming from the brainstem. The impaired brainstem-sensorimotor connection might be, Barnden thought, impacting motor functioning in ME; i.e. the ability to carry out physical activity.Signals to move muscles pass from the motor cortex to the sensorimotor cortex down to the thalamus and then through the brainstem to the muscles. (Signals from the muscles to the brain pass up through the same pathways.) Barnden proposed that the movement problems in ME/CFS could start with the brainstem's inability to properly relay signals to the motor cortex to activate the muscles.Barnden's most recent brainstem study validated the idea that inadequate communication between the brainstem nuclei and other nuclei in the brain, including the vasomotor region, hypothalamus and prefrontal cortex, was affecting autonomic nervous system functioning in ME/CFS.
Another study finding of impaired communication from the brainstem nuclei to other nuclei in the brain suggested the same, and found increased signs of myelination in the sensorimotor cortex of the brain. Barnden proposed that decreased signaling from a damaged brainstem provoked a compensatory increase in myelination in the sensorimotor region as it bulked up to try to understand the limited signaling coming from the brainstem. The impaired brainstem-sensorimotor connection might be, Barnden thought, impacting motor functioning in ME; i.e. the ability to carry out physical activity.Signals to move muscles pass from the motor cortex to the sensorimotor cortex down to the thalamus and then through the brainstem to the muscles. (Signals from the muscles to the brain pass up through the same pathways.) Barnden proposed that the movement problems in ME/CFS could start with the brainstem's inability to properly relay signals to the motor cortex to activate the muscles.Barnden's most recent brainstem study validated the idea that inadequate communication between the brainstem nuclei and other nuclei in the brain, including the vasomotor region, hypothalamus and prefrontal cortex, was affecting autonomic nervous system functioning in ME/CFS.
Other Kinds of Brain Scans
Other kinds of brain scans, such as magnetic resonance spectroscopy (MRS), can pick up signs of neuroinflammation. Although almost 10 MRS studies of the brain in ME/CFS have been done, VanElzakker et. al. report that a clear and consistent picture of metabolite alterations in the brain has yet to emerge.They believe that's due largely to a common theme in medical research, found in this disease in particular - lack of standardization. Different diagnostic criteria, different types of healthy controls, different brain regions examined, and different metabolites targeted make it difficult to present a clear picture of the metabolic alterations in the brains of people with ME/CFS.
The Japanese Take
The Japanese probably couldn't agree with Barnden more. Their studies indicate that, as the healthy controls became more fatigued, two core regions - both of which communicate with the brainstem ( the prefrontal cortex and the anterior cingulate cortex) - shut down.As these regions begin to shut down, control of autonomic functioning becomes lost. In particular, the ability to activate the parasympathetic nervous system (i.e. the vagus nerve) and tone down the sympathetic nervous system activity, is lost.The Japanese believe a breakdown in what they call the facilitation system in the brain has occurred. As we become fatigued, the facilitation system jumps in to increase the signals coming from the primary motor cortex to the muscles. This increased “drive” from the motor cortex prompts the muscles to work harder and activates more and more of them so that activity can proceed.https://www.healthrising.org/blog/2016/05/31/fatigue-japanese-way/So long as new, fresh muscle fibers remain to be recruited, the activity can continue. If no muscle fibers are left to be recruited or if the brain has a problem recruiting new muscle fibers, fatigue sets in.A 2003 study suggested that reduced muscle recruitment due to reduced motor cortex output was indeed occurring in ME/CFS. That study suggested that, “… changing motor deficits in CFS has a neurophysiological basis [which] … supports the notion of a deficit in motor preparatory areas of the brain”. That study titled, “Deficit in motor performance correlates with changed corticospinal excitability in patients with chronic fatigue syndrome“, to my knowledge was never followed up on.https://www.healthrising.org/blog/2014/09/03/fatigue-explained-japanese-brain-damage-chronic-fatigue-syndrome/
Conclusion
Several studies suggest significant brainstem issues may be present in ME/CFS. Problems with the brainstem could produce everything from autonomic nervous system problems to immune issues to problems with movement.The authors critique past brain imaging studies and provide a "how to" guide to assess the brainstem in ME/CFS. Barnden's Australian brainstem studies suggest that when done correctly, MRI imaging studies may indeed find extensive damage is present in ME/CFS including evidence of brainstem neuron demyelination, a compensatory remyelination in parts of the brain the brainstem connects with, and lastly, a reduced connectivity between these regions.VanELzakker et. al. assert that future imaging studies that focus on the specific functional connectivity pathways in the brain which are activated by inflammatory processes should be able to capture the neuroinflammatory processes occurring in ME/CFS. (Two of the three pathways they cite include the brainstem.) The thalamus's role in sensory stimuli activity presents another fruitful pathway to assess. Lastly, the authors suggest that researchers target the nucleus of the solitary tract (NTS) where the vagus nerve enters the brainstem.With help from an ME/CFS donor, VanElzakker has been employing brain imagining techniques to assess the brainstem in chronic fatigue syndrome (ME/CFS). He will be speaking at the NIH ME/CFS Conference in Baltimore in April.http://simmaronresearch.com/2013/12/one-theory-explain-vagus-nerve-infection-chronic-fatigue-syndrome/
