The First ME/CFS Fecal Transplant Study Suggests the Treatment Holds Promise
Finally a (chronic fatigue syndrome) ME/CFS fecal transplant study. It's long past due (Maybe way, way long past due - the Chinese pioneered fecal transplants 2000 years ago but used a cruder method in people dying of diarrhrea - drinking them.)This first stab at a fecal transplant study isn't a big statistically rigorous, randomized, placebo-controlled trial. Far from it; it's more a series of case reports from a physician's practice over time with a smattering of statistics. It does give us, though, our first data -in rather vivid detail - on the possible efficacy of fecal transplants in ME/CFS. Ten studies now indicate that the bloom is off in the gut flora of people with ME/CFS. With a 2018 review taking ME/CFS researchers to task for the usual suspects: lack of standardization in patient selection, sample processing, genome sequencing and data analysis, it's not clear what has gone wrong.As papers just pour out implicating the gut flora in a wide range of diseases the question becomes more and more what to do about it. While pre and probiotics can help, it's possible that fecal transplants - the direct transfer of stool (or portions of the stool) from a healthy person into the gut of an ill person - may provide a larger, more lasting impact.
Ten studies now indicate that the bloom is off in the gut flora of people with ME/CFS. With a 2018 review taking ME/CFS researchers to task for the usual suspects: lack of standardization in patient selection, sample processing, genome sequencing and data analysis, it's not clear what has gone wrong.As papers just pour out implicating the gut flora in a wide range of diseases the question becomes more and more what to do about it. While pre and probiotics can help, it's possible that fecal transplants - the direct transfer of stool (or portions of the stool) from a healthy person into the gut of an ill person - may provide a larger, more lasting impact.
The Study
Dr. Julian Kenyon runs The Dove Clinic for Integrated Medicine, in the U.K. which uses both an oral (pre and probiotics, diet, etc.) and fecal transplant approach to gut improvement. In this study - A Retrospective Outcome Study of 42 Patients with Chronic Fatigue Syndrome, 30 of Whom had Irritable Bowel Syndrome. Half were treated with oral approaches, and half were treated with Faecal Microbiome Transplantation - he compared the results of the two.Kenyon divided his patients into two groups of 21; one was treated with nutritional remedies, probiotics, prebiotics, and dietary and lifestyle advice. The second group, most of whom had failed the first treatment approach, were given 10 fecal implants over ten days.As seventy percent of the group also had irritable bowel syndrome (IBS) this may have been a more gut impacted group. In an effort to deliver a maximum diversity of flora, each of the implants came from a different, "carefully screened" donor.The Taymount Laboratory provided the implants. The laboratory runs a 10-day gut flora transplant (FMT) program which starts off with a colon cleanse and includes dietary advice.While it's not possible to test donors for all possible pathogens (some of which may be undetectable), the donors' blood was screened for the following pathogens: Human Immunodeficiency Virus (HIV) 1/2, Hepatitis A. IgM, Hepatitis B (HBsAg), Hepatitis C antibody, Syphilis, IgG/IgM, Full Blood Count, Urea and Electrolytes, Ferritin, C-Reactive Protein, Tissue Transglutaminase, CMV, H-Pylori.Their stool samples were screened for: Campylobacter (Jejuni, Coli and Upsalliensis), Clostridium Difficile (A/B), Salmonella, Yersinia Enterocolitica, Vibrio (Parahaemolyticus Vulnificus and Cholera), Diarrhoea-causing E-Coli/Shigella, Enteroaggregative E-Coli (EAC), Enteropathogenic E-Coli (EPEC), Enterotoxigenic E-Coli (ETEC), Shiga-like toxin-producing E-Coli (STEC), E-Coli 0157, Shigella/Enteroinvasive E-Coli (EIEC), Cryptosporidium, Cyclospora Cayetanesis, Entamoeba Hystolitica, Giardiolambia, Adenovirus, Astrovirus, Norovirus GI/GLL, Rotavirusa, Sapovirus.The Taymount Laboratory website reports that there's no documented evidence infections being passed via fecal transplants. As of this month, though, that's no longer true. The FDA recently reported on two multi-drug resistant infections passed via fecal transplants.Different kinds of transplant techniques are used. Some clinics use a tube to insert the transplant through the esophagus and into the stomach or the duodenum. This clinic uses a rectal catheter to deliver the goodies into the large bowel or colon. Others use something called a colonoscope. Some companies are creating pills that can be swallowed.
Results
The study reported on past patient outcomes (retrospective case-control) using a vague metric indeed, "% improvement", to assess results. While the statistics were crude, the data presented - in short statements describing how the patients improved or didn’t improve - provided vivid reading indeed.The statistics (Mann-Whitney test of "% improvement: U=111.5, p=.003) indicated dramatically increased improvements in the fecal transplant group compared to the "oral" (probiotic, nutritional supplements, etc.) group.
The Fecal Transplant Group
As noted above the fecal transplant group were tough cases: they hadn't responded to Dr. Kenyon's normal treatment regiment of supplements, pre and pro-biotics etc.Dr. Kenyon's data suggested that little grey area existed: the fecal transplants either hit or missed: when they hit, they tended to work quite well; when they missed, they pretty much missed entirely.In quite a few cases, the transplants were associated with some striking increases in energy. Kenyon reported that the energy levels of 7 of the fecal transplant group returned to normal, practically normal or almost normal. (In one case she simply said "chronic fatigue syndrome resolved".)The increases in energy did not come in the newly ill either. Six people who'd had ME/CFS "for many years" either totally recovered or were dramatically improved. One 66 year old person who apparently got ill following an amoebiasis infection in the Himalayas over 30 years ago returned to normal health.The energy levels of six others were "significantly improved", "much improved", "improved dramatically" or "consistently improved".In a few cases, it was impossible to determine if improvements in energy had occurred. For instance, Dr. Kenyon reported that the gut problems of a person with severe vaginal thrush, recurrent abdominal bloating, IBS and ME/CFS largely disappeared but didn’t assess her energy levels. The same occurred with another person with IBS: their IBS disappeared but we weren't told if her energy levels improved as well.Four people (@20%) were either unable to tolerate the implants (n=2) or showed no improvement (n=2).Table 1. Chronic Fatigue Syndrome Patients treated with FMT
| Patient: | %Improved | |
| (F)Age 36 | Severe Chronic Fatigue Syndrome with Irritable Bowel Syndrome for three years, following multiple antibiotics for Quinsy. Severe debilitating Irritable Bowel, with lack of energy. She had FMT in February 2018, following this the Irritable Bowel cleared up, energy significantly better. Has always had many food sensitivities, they are gradually beginning to resolve. A further course of FMT is under consideration. | 70% |
| (F)Age 40 | Polycystic Ovary Syndrome, also Irritable Bowel and a Chronic Fatigue. She had FMT in October 2017, following the FMT her energy is much improved and is practically normal, has remained so ever since. Also, her mood is more stable. | 90% |
| (F)Age 59 | Severe Vaginal Thrush for five years, recurrent abdominal bloating, Irritable Bowel Syndrome and Chronic Fatigue Syndrome. Clostridium Difficile in 2013. She had FMT in May 2017, two months after FMT the Irritable Bowel cleared up completely, her skin is significantly better than it was prior to treatment, Vaginal Thrush is still something of a problem, but not as bad as it was. She finds she is no longer craving sweet foods. | 90% |
| (F)Age 73 | History over many years of Irritable Bowel Syndrome and Chronic Fatigue Syndrome, also overweight. We treated her with FMT in December 2017, the Irritable Bowel Syndrome cleared up during the two months following the FMT and has remained normal. She is still having difficulty in losing weight. | 60% |
| (F)Age 43 | Several years history of Chronic Fatigue Syndrome. Also, Irritable Bowel Syndrome. We carried out FMT in January 2017, since that time the IBS has cleared up, energy significantly improved and has remained so. | 70% |
| (F)Age 42 | 8-year history of Chronic Fatigue Syndrome. Also, Irritable Bowel Syndrome. We treated her with FMT in November 2018, I first saw her in May 2018. Since the FMT her persistent Oral Thrush has cleared, her digestion has improved, and the Irritable Bowel has settled down. She is no longer constipated. Her energy improved almost to normal following the FMT but has had a bit of a relapse since significant family upset, which has been draining on her energy reserves. | 95% |
| (F)Age 73 | Insomnia, persistent Nausea, poor energy due to Chronic Fatigue Syndrome, lack of appetite. Has lost a great deal of weight over several years. Complains of bad body odour. We carried out FMT in February 2017. Since then the Nausea has disappeared, the appetite has returned, and she is now putting on weight. | 95% |
| (F)Age 46 | I first saw her in 2016 with a history of Chronic Fatigue Syndrome and Fibromyalgia for several years. We carried out FMT in January 2017, no significant response to the FMT. We are thinking of repeating the FMT. | 0% |
| (F)Age 66 | At the age of 26 this patient contracted amoebiasis in the Himalayas, then she had lots of antibiotics for various indications and has had Irritable Bowel Syndrome and Chronic Fatigue Syndrome since the age of 30. Also, she has been diagnosed with SIBO and had developed multiple food sensitivities. We carried out FMT in July 2017, her Irritable Bowel Syndrome normalised over the next four weeks, her energy improved and became normal, then she had exposure to contaminated water, probably containing parasites, then she relapsed to some extent and had to have a second course of FMT in December 2017. Since that time, she has been completely normal. | 95% |
| (F)Age 47 | This patient has had regular courses of antibiotics since the age of 12 for a range of reasons. She has had many years of Chronic Fatigue and Irritable Bowel Syndrome. We carried out FMT in August 2018, since then the Irritable Bowel has settled down and the Chronic Fatigue has resolved. | 90% |
| (F)Age 73 | This patient has had a history of recurrent Candidiasis over many years, including Oral Thrush. She has many years history of Irritable Bowel Syndrome and Chronic Fatigue Syndrome. We carried out FMT on her in November 2018. Since that time, she has had no more Candidiasis, the Irritable Bowel has settled down, and there is significant maintained improvement in her energy levels. | 85% |
| (F)Age 70 | This patient has had a history over many decades of a Chronic Fatigue Syndrome. We used FMT in April 2017, there was no improvement in her energy levels since the FMT. | 0% |
| (F)Age 70 | Chronic Fatigue Syndrome for 20 years, also Addison’s Disease, Fibromyalgia and Irritable Bowel Syndrome. FMT carried out in August 2018. She reacted to several of the Implants with Diarrhoea, so we had to stop the Implants. Clinically, no change. | 0% |
| (F)Age 61 | 20-year history of Chronic Fatigue Syndrome and Fibromyalgia, also Irritable Bowel Syndrome. Oral treatment did not work. FMT was carried out in April 2018. Following FMT her energy improved dramatically and has remained improved. The Irritable Bowel Syndrome has cleared up and she also lost one and a half stone in weight. | 90% |
| (F)Age 41 | Many years history of Chronic Fatigue Syndrome, multiple food sensitivities and Irritable Bowel Syndrome. FMT carried out in September 2018. She managed to tolerate half of the Implants and then temporarily had to stop. No clinical improvement yet. | 0% |
| (F)Age 44 | Eight-year history of Chronic Fatigue Syndrome getting significantly worse. Also, Irritable Bowel Syndrome. We carried out FMT on her in October 2018. Her Irritable Bowel Syndrome has cleared up completely, energy is beginning to recover. | 75% |
| (F)Age 56 | History of Chronic Fatigue Syndrome, Irritable Bowel Syndrome for many years. Resistant to oral approaches for treating both of these conditions. We carried out FMT in May 2018. Since that time her energy is significantly better, and remains better, bowel function is now normal. | 80% |
| (F)Age 70 | Chronic Fatigue Syndrome for many years, also Irritable Bowel Syndrome. We treated her with FMT in October 2017. Bowel habit is now normal, resistance to intercurrent infections has now returned to normal, energy was consistently improved and remains so. | 95% |
| (M)Age 65 | Chronic Fatigue Syndrome for many years. We treated him with FMT in November 2017. Energy has returned to normal. | 95% |
| (F)Age 52 | This patient has had Chronic Fatigue Syndrome for many years. Also, Irritable Bowel Syndrome. We treated her with FMT in July 2018. Since then, her energy has returned to normal and she has now been able to return to work, her gut has also returned to normal. | 95% |
| (F)Age 48 | History of Chronic Fatigue Syndrome and Irritable Bowel for many years. We carried out FMT on her in March 2018. Since then her Irritable Bowel Syndrome has cleared up completely and also her energy has returned to normal. | 95% |
The Standard or Oral Approach Group
The other group treated with nutritional remedies, probiotics, prebiotics, and dietary and lifestyle advice generally did improve - but not nearly to the extent that the fecal transplant group did.Dr. Kenyon reported that most had improved by 30-40% (N=10), two people - one who had had ME/CFS for decades but improved rapidly on Dr. Kenyon's regimen - improved by 90%, two by 50-75% and the rest with lesser improvements.Dr. Kenyon, not surprisingly, concluded that fecal transplants are more effective at repairing gut flora than pre and probiotics. While two people responded poorly to the transplants, Kenyon reported they generally provide a safe and potentially effective approach to ME/CFS.
Fecal Transplants
That begs the question - just exactly what is a fecal transplant? It turns out that a variety of transplants are done. Some transplants transfer all the fecal matter while others filter out other components and only transfer the bacteria.The Taymount Clinic reported that they implant only bacterial matter. People who go the home route obviously transfer everything: get poop from a healthy donor, and then use saline solution and an enema to get the poop in (which they hold for as long as possible).As might be imagined raw fecal matter contains all sorts of substances of which bacteria make up just one component. Generally about 75% water and 25% solid matter, bacteria make up between 25-55% of the solid matter and 6-13% of the total matter. That's a lot of bacteria - approximately one hundred billion per gram of wet stool - although only 3.0%–6.6% of total fecal matter may be composed of viable bacteria.
Some History
Other components found in fecal matter include significant numbers of epithelial cells that have flaked off the colon (colonocytes), single-celled organisms call archeae and other primitive organisms, viruses, fungi and metabolites.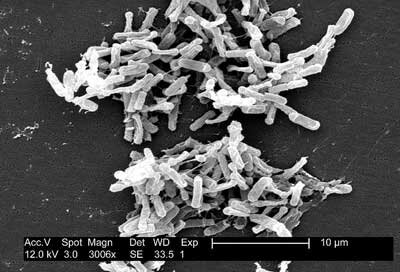 In the U.S.. fecal transplants have mostly been used to battle life-threatening Clostridium difficile infections. Transplants got a boost in early 2000's after a particularly virulent form of C. difficile hit the U.S., causing gastroenterologists and patients to scramble for more effective treatments. Six hundred and twenty-five thousand C. difficile cases are believed to occur in the U.S and Europe every year.One women's unstoppable C. difficile infection prompted her gastroenterologist to tell her, after seven months, to get her affairs in order. She ended up using her daughter as a donor in 2014. She reported:
In the U.S.. fecal transplants have mostly been used to battle life-threatening Clostridium difficile infections. Transplants got a boost in early 2000's after a particularly virulent form of C. difficile hit the U.S., causing gastroenterologists and patients to scramble for more effective treatments. Six hundred and twenty-five thousand C. difficile cases are believed to occur in the U.S and Europe every year.One women's unstoppable C. difficile infection prompted her gastroenterologist to tell her, after seven months, to get her affairs in order. She ended up using her daughter as a donor in 2014. She reported:
"My gut drank up the infusion as if it were dying of thirst. My colon, after five months of near-constant spasms, recovered in one transformative instant. Overnight, I went from having 30 bowel movements a day to having one. For breakfast the next morning, I ate a quesadilla loaded with black beans, cheese, salsa, lettuce, and guacamole. I’ve had no recurrence of C. diff. since."
Four pharmaceutical companies in the U.S. reportedly provide stool donors to doctors - mostly for C. difficile infections. In 2016 the FDA's decision to require stool banks to provide an expensive investigational new drug application (IND) in order to provide stool resulted in the agency being accused of erecting barriers to treatment which would result, among other things, in more unregulated, home use. Other less restrictive measures were proposed.Although it's believed that tens of thousands of fecal transplants have been done safely, the FDA recently reported for the first time that multi-drug resistant infections were transferred via fecal transplants to two people one of whom had died. The death occurred in a man with a compromised immune system who had been given a transplant which had not been screened for a type of resistant E. coli,. As a result, as of July 15th of this year, the FDA is requiring stool transplant companies to screen their poop for a variety of multi-drug resistant organisms.
Conclusion
The first stab at a fecal transplant study in ME/CFS was weak in statistics and strong in vivid detail. Dr. Kenyon's fecal transplants - used mostly in ME/CFS plus IBS patients - used only bacterial matter and were done in bulk - ten transplants over ten days - from different donors to ensure that a wide variety of flora was transmitted.With seven of the 21 treatment resistant patients reportedly returning to full or near normal health, and six receiving significant improvements in energy, the results were surprisingly good.While the results were promisingly we need more rigorous studies and one, funded by Invest In ME and lead by Peter Johnsen, a Norwegian researcher is underway. Data collection from the 80 person, randomized, placebo-controlled study at the University Hospital of North Norway started in February of this year and is slated to wind up in February of next year. I couldn't tell how many fecal transplants would be given but changes in gut microbiome, metagenome, metabolome, gut barrier integrity and immune functioning will be assessed at three time points during the year long study.Johnsen's 2018 (n=86) study found that fecal transplants "provided significant symptom relief for people with IBS. (In a nice bit of collaboration Maureen Hanson will be testing some of Johnsen's samples for gut dysbiosis.)
