Solid Ground at Last? Cytokines Make Good in Major ME/CFS Review
The immune system in chronic fatigue syndrome (ME/CFS) has been kind of like a mirage in the desert. Given the way the disease starts and its symptom presentation - so close to the "sickness behavior" produced during an infection - it seems that the immune system must be a major player in this illness. Like a mirage in the desert, though, the powerful drivers of the immune system - the cytokines - seem to slip through our grasp again and again. Interesting findings pop only to be dashed by another study.Thirty plus years of study have left us - according to several immune reviews - with precious little solid ground. A recent review, however, suggested that larger studies were finally producing more consistent results.Now we have the largest "study" of all - a meta-review of past cytokine (inflammatory protein) studies - that's providing us a solid foundation, and from the unlikeliest of places, Kings College in the U.K., which has been better known as a bastion of cognitive behavioral therapy.The senior author of the paper, the rather prolific Anthony Cleare, has focused for years on the HPA axis in ME/CFS. He and the lead author, Rebecca Strawbridge, have shared an interest in the role inflammation plays in HPA axis issues and depression. Strawbridge's recent paper on the effectiveness of anti-inflammatories in depression clearly underscored how often inflammation instead of psychology is driving depression.Their new paper's rather emphatic title "Inflammatory proteins are altered in chronic fatigue syndrome-A systematic review and meta-analysis" seemed to give notice that things had changed. ME/CFS is, at least in part, an inflammatory disease after all.The review was broad: any diagnostic criteria was allowed and the main exclusionary criteria was that no stimulation of any kind was involved; i.e. this was an assessment of the immune system at rest. The 42 studies involved highlight just how hard researchers in this small field have searched for an immune cause of ME/CFS.The authors of the present paper pointed out why the immune system has been such a draw for this field. "Phenomenologically" they noted, "ME/CFS is often described as a ‘flu-like illness’ and the diagnostic criteria to some extent resemble the symptoms of sickness behaviour." (Sickness behavior describes the symptoms produced by the brain during infection (fatigue, pain, cognitive problems, etc.) that serve to isolate an individual from the community - and thus help stop the spread of a pathogen).
Like a mirage in the desert, though, the powerful drivers of the immune system - the cytokines - seem to slip through our grasp again and again. Interesting findings pop only to be dashed by another study.Thirty plus years of study have left us - according to several immune reviews - with precious little solid ground. A recent review, however, suggested that larger studies were finally producing more consistent results.Now we have the largest "study" of all - a meta-review of past cytokine (inflammatory protein) studies - that's providing us a solid foundation, and from the unlikeliest of places, Kings College in the U.K., which has been better known as a bastion of cognitive behavioral therapy.The senior author of the paper, the rather prolific Anthony Cleare, has focused for years on the HPA axis in ME/CFS. He and the lead author, Rebecca Strawbridge, have shared an interest in the role inflammation plays in HPA axis issues and depression. Strawbridge's recent paper on the effectiveness of anti-inflammatories in depression clearly underscored how often inflammation instead of psychology is driving depression.Their new paper's rather emphatic title "Inflammatory proteins are altered in chronic fatigue syndrome-A systematic review and meta-analysis" seemed to give notice that things had changed. ME/CFS is, at least in part, an inflammatory disease after all.The review was broad: any diagnostic criteria was allowed and the main exclusionary criteria was that no stimulation of any kind was involved; i.e. this was an assessment of the immune system at rest. The 42 studies involved highlight just how hard researchers in this small field have searched for an immune cause of ME/CFS.The authors of the present paper pointed out why the immune system has been such a draw for this field. "Phenomenologically" they noted, "ME/CFS is often described as a ‘flu-like illness’ and the diagnostic criteria to some extent resemble the symptoms of sickness behaviour." (Sickness behavior describes the symptoms produced by the brain during infection (fatigue, pain, cognitive problems, etc.) that serve to isolate an individual from the community - and thus help stop the spread of a pathogen).
The Review
The vast majority of studies used either the Fukuda or the 1994 criteria created by the CDC. Both criteria have been mostly discarded in favor of more recent criteria but it should be noted that most ME/CFS studies - including many with positive outcomes - used one or other of these definitions. (Only 8 of the 42 studies used the Canadian or International criteria - which may have issues of their own.)Despite the broad criteria (Oxford definition, CDC definitions included) used in most of the studies, this meta-review actually found evidence for an inflammatory state in ME/CFS. The authors hypothesized that pro-inflammatory cytokines and acute phase protein levels would be significantly higher in people with ME/CFS than controls, and low and behold, they were.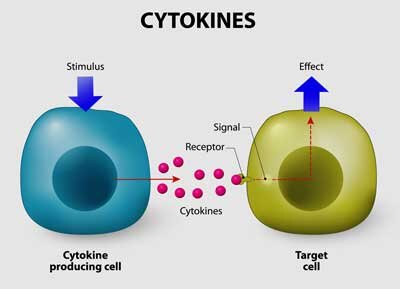 Approximately 22 cytokines/immune factors were assessed in 42 studies dating from 1989 to 2016. The review suggested that about a quarter of the immune factors assessed in ME/CFS were elevated.Elevations of two cytokines (tumor necrosis factor-a (TNF-a), c-reactive protein (CRP)), both of which have wide ranging effects, suggested that ME/CFS was similar to other "chronic immune conditions" which have a similar cytokine profile.
Approximately 22 cytokines/immune factors were assessed in 42 studies dating from 1989 to 2016. The review suggested that about a quarter of the immune factors assessed in ME/CFS were elevated.Elevations of two cytokines (tumor necrosis factor-a (TNF-a), c-reactive protein (CRP)), both of which have wide ranging effects, suggested that ME/CFS was similar to other "chronic immune conditions" which have a similar cytokine profile.
Synchronicity
A recent gene expression study highlighted both TNF-a and TGF-B as well. In fact, that study identified precise pathways associated with TNF-a which might potentially be targeted in ME/CFS. The fact that these cytokines are popping up in independent studies suggests we may finally be honing in on some key cytokines that are producing fatigue, pain and other symptoms in ME/CFS.http://simmaronresearch.com/2019/11/pathways-fine-tuning-treatments-chronic-fatigue-syndrome/Cytokines involved in regulating inflammation ((IL-2, IL-4 and TGFβ) appeared to be particularly affected. Three cytokines (IL-6, IL-1 and IL-12) involved in the early response to infection (perhaps suggesting viral reactivation was present) tended to be increased as well but were less consistently elevated. Interestingly, given the hypothesis that immune exhaustion occurs over time in ME/CFS, no trends in reduced cytokine levels were found.
Capturing Smoke in a Bottle
The authors noted that some similar (but different) findings have been found in fibromyalgia and depression, and that given the widespread co-occurrence of all three disorders teasing what is caused by what is tricky. Noting that fatigue is found in both ME/CFS and depression, and that inflammation can produce "disabling fatigue", the authors suggested future studies more clearly delineate the extent of depression present. Activity levels and medication use - both of which can affect the HPA axis or immune system should be characterized. .The review also noted, as did Van Elzakker's rather scathing recent review of cytokine studies, that measuring cytokines is a bit like capturing smoke in a bottle. Their levels fluctuate constantly and can be effected by activity levels, diet, medication use, weight, age, sex and "numerous other factors".For instance, it's clear that activity levels, diet, medication use - all factors which could skew cytokine findings - will probably be different in ME/CFS patients. Therefore, they could by themselves account for the altered levels found. Plus a bunch of other factors (severity and duration of illness, illness triggers, illness history, sample collection, processing, storage) could all tweak cytokine levels.Given that few ME/CFS studies accounted for most of these factors (and mostly used outdated criteria) it seems remarkable that the review found consistent results at all.
A Plea for A Cytokine Study (To End All Cytokine studies)
Once again, for the umpteenth time it seems, the authors left us with a plea for larger, more rigorously controlled studies. The authors, in fact, recommended what sounded like a cytokine study to end all cytokine studies. That study would subgroup patients, assess all confounding factors and then follow the patients over time (longitudinal study). A very large study using the best criteria available could tease out definitive immune biomarkers and pave the way for potential treatments. The increasing number of biologic drugs being developed to target specific cytokines make that drug arena a potentially very fruitful one for ME/CFS.Dr. Klimas is certainly on board. Her Enbrel (plus mifepristone) trials in ME/CFS and GWI indicate she thinks she's already found a target. Enbrel, interestingly, targets TNF-a - one of the cytokines the review found elevated in ME/CFS.Breaking their British reserve a bit at the very end of the paper, the authors stated they "fervently" await better studies so that they can conduct a more comprehensive meta-analysis- and better understand the role that inflammatory proteins play in ME/CFS.One wonders if we could be just one or two very big, rigorous and comprehensive cytokine studies away from identifying an FDA-approved drug that could help many. This review will surely provide support for studies like that.
A very large study using the best criteria available could tease out definitive immune biomarkers and pave the way for potential treatments. The increasing number of biologic drugs being developed to target specific cytokines make that drug arena a potentially very fruitful one for ME/CFS.Dr. Klimas is certainly on board. Her Enbrel (plus mifepristone) trials in ME/CFS and GWI indicate she thinks she's already found a target. Enbrel, interestingly, targets TNF-a - one of the cytokines the review found elevated in ME/CFS.Breaking their British reserve a bit at the very end of the paper, the authors stated they "fervently" await better studies so that they can conduct a more comprehensive meta-analysis- and better understand the role that inflammatory proteins play in ME/CFS.One wonders if we could be just one or two very big, rigorous and comprehensive cytokine studies away from identifying an FDA-approved drug that could help many. This review will surely provide support for studies like that.